![]() Dispersing Wellness
Dispersing Wellness
Fall 2019
Columbia University Graduate School of Architecture, Planning and Preservation
Urban Design Studio
Location
Hudson Valley
Regional Scale
Critics
Kaja Kuhl; Anna Dietzsch, Justin G. Moore, Jerome Haferd, Liz McEnaney, Shachi Pandey, Raafi Rivero, David Smiley, Dragana Zoric
Team
Niharika Shekhawat, Mansoo Han, Ting Zhang, Shailee Shah
The goal of the project is to substantially lower the carbon footprint and reduce health disparities within the urban/rural context by dispersing wellness through social infrastructure in the Hudson Valley. Within the healthcare industry, 84% of CO2 comes from health system supplies and services and 16% from the building facilities itself. The idea is to change the perspective of health services. Hospital acts as a promoter of community well being in urban area and disperses wellness through additive typologies of social infrastructure in rural areas. The project challenges and changes the perspective of the current healthcare system from being a measure of cure to an extension of health and wellbeing of the community. The goal of the project is to substantially lower the carbon footprint and reduce health disparities within the urban/rural context by dispersing wellness through social infrastructure in the Hudson Valley.
The healthcare industry accounts for 10% of the total greenhouse gases generated. We have two major issues that are often ignored of the healthcare system - High carbon footprint and lack of accessibility(physical and monetary) that in turn makes people sicker and more dependent on health facilities in the long run. The healthcare facilities provide health services but are high polluters of the environment, in turn making people sicker and more dependent on health facilities in the long run. Another cycle is the lack of physical and monetary access to healthcare that makes people conditioned to living with the discomfort of disease which further enhances the gap as it propels them to get treated only in “when needed” scenario with high expenditure.
The GND aims to focus on “Providing all people of the United States with high quality health care” However, the measures do not solve for the high carbon footprint of healthcare and the accessibility factor.Of the total greenhouse gases generated in the USA, 84% of emissions in the industry are derived from manufactured products used in healthcare delivery as well as the energy and transportation required to acquire them while the other 16% of the gas emissions derive from the building systems of health facilities. Therefore, we understand that a large percent of emissions can be reduced through patient preventative healthcare and supporting measures that would make people healthier.
The healthcare industry accounts for 10% of the total greenhouse gases generated. We have two major issues that are often ignored of the healthcare system - High carbon footprint and lack of accessibility(physical and monetary) that in turn makes people sicker and more dependent on health facilities in the long run. The healthcare facilities provide health services but are high polluters of the environment, in turn making people sicker and more dependent on health facilities in the long run. Another cycle is the lack of physical and monetary access to healthcare that makes people conditioned to living with the discomfort of disease which further enhances the gap as it propels them to get treated only in “when needed” scenario with high expenditure.
The GND aims to focus on “Providing all people of the United States with high quality health care” However, the measures do not solve for the high carbon footprint of healthcare and the accessibility factor.Of the total greenhouse gases generated in the USA, 84% of emissions in the industry are derived from manufactured products used in healthcare delivery as well as the energy and transportation required to acquire them while the other 16% of the gas emissions derive from the building systems of health facilities. Therefore, we understand that a large percent of emissions can be reduced through patient preventative healthcare and supporting measures that would make people healthier.
Winner of Radical Urban Intervention 2020 ArcDeck.net
(Student Category)
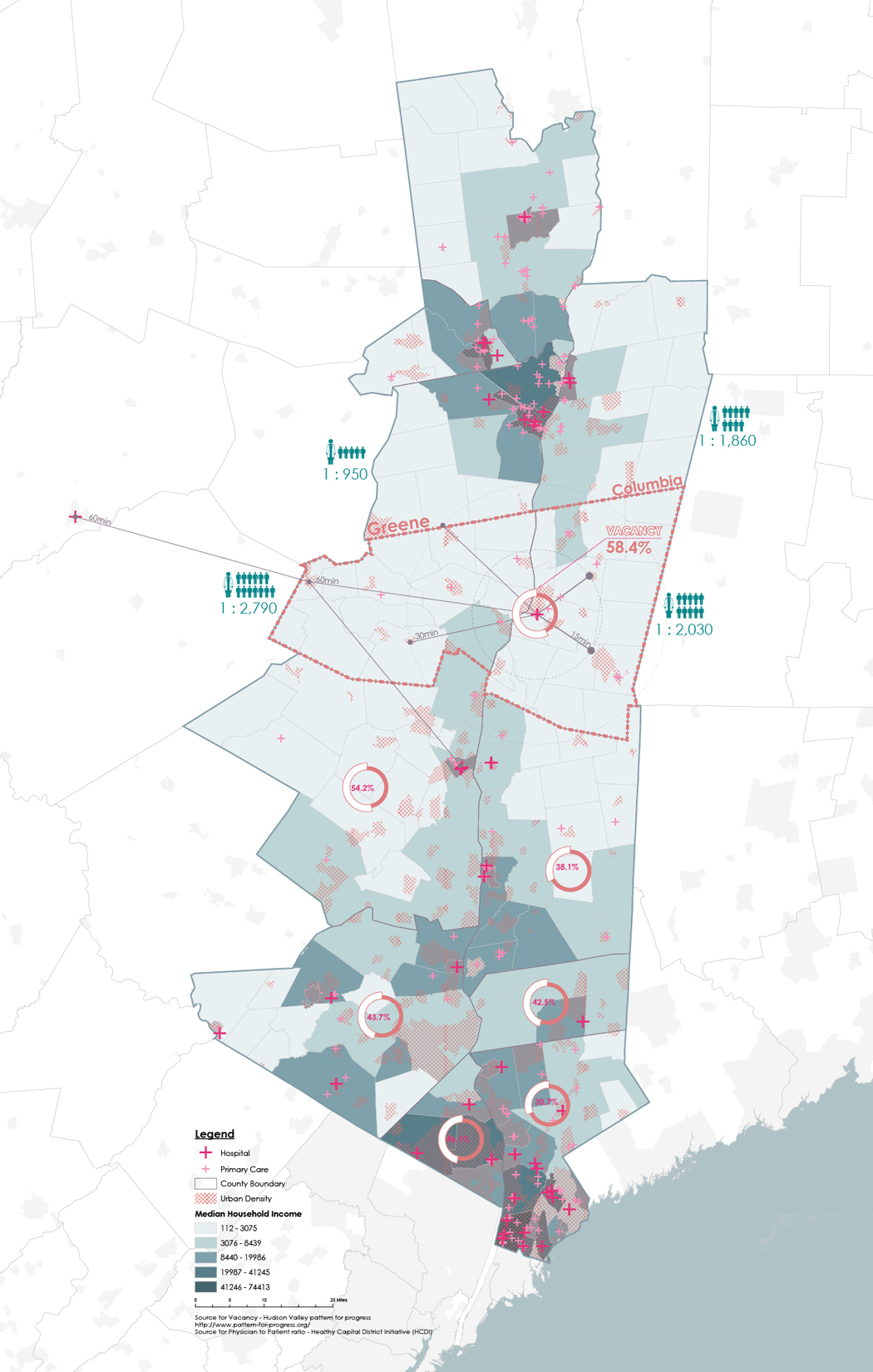
Map of the Hudson Valley showing concentration of hospitals in Urban Areas.
In the Hudson Valley, we see that the concentration of hospitals in urban areas is much higher whereas the rural areas lack services to healthcare. Therefore, there is a huge health care disparity in terms of accessibility between the urban and rural areas. The base maps represents median household income, we see that the areas that have higher income have more access to health facilities whereas low income, which are more rural areas lack health facilities completely. The geography of the region drives people’s health seeking behavior in Hudson Valley, residents especially from the rural areas are the most disadvantaged and travel upto 1.5 hours one way for basic health needs. At the same time, within the Hudson valley, hospitals show at least upto 30% percent vacancy of beds in each county, areas that can be more efficiently repurposed.
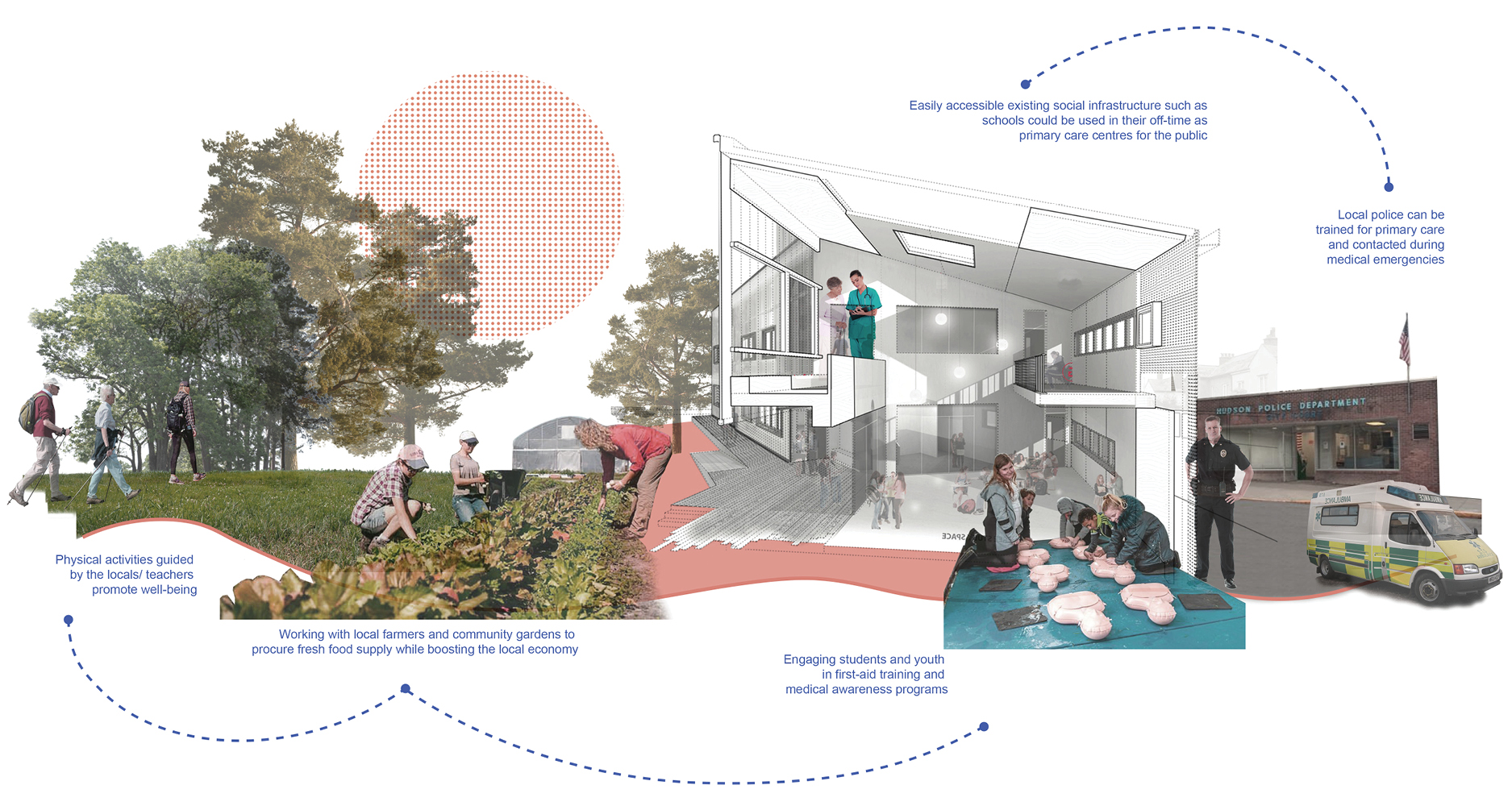
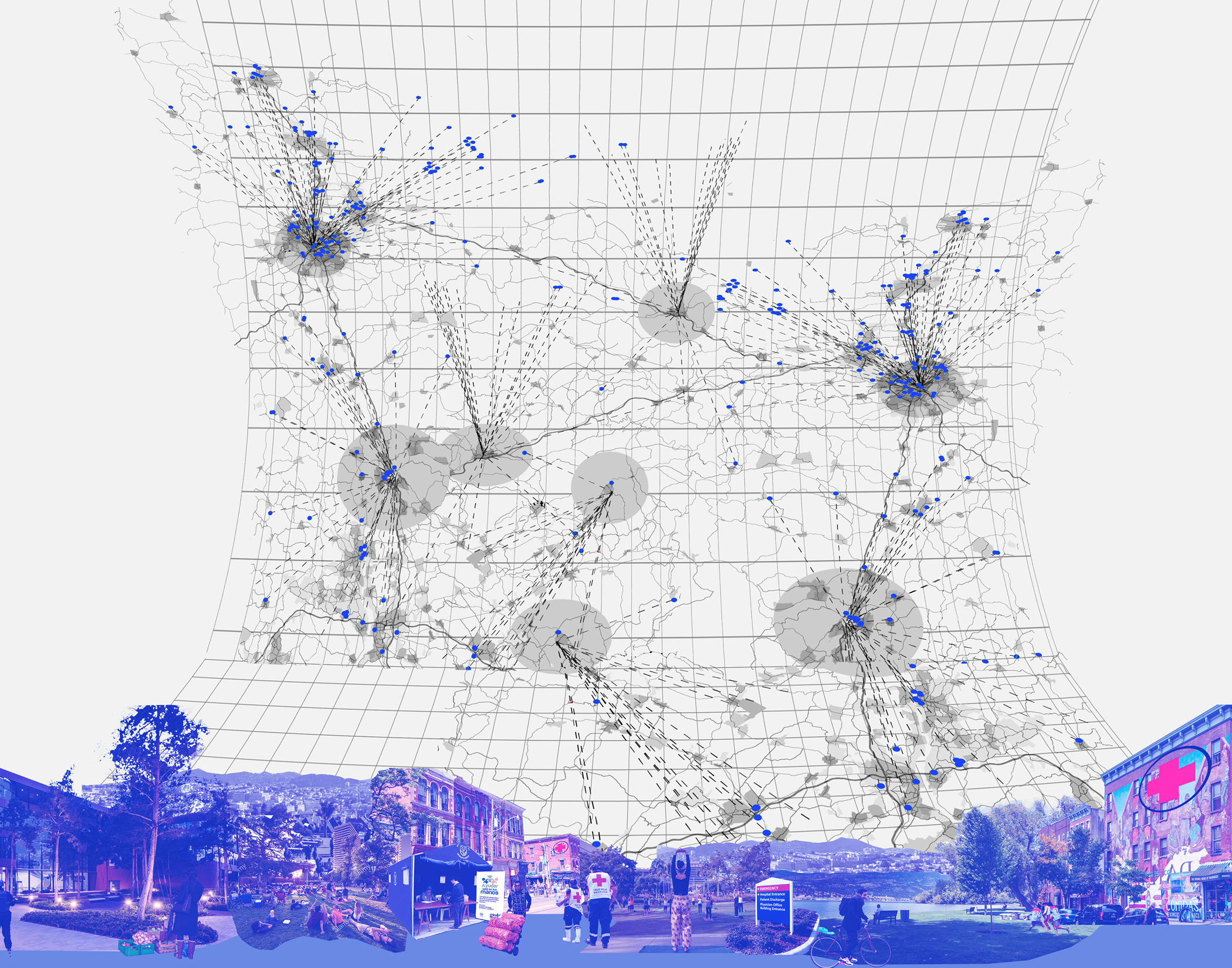 Visual collage of extension of health services in the rural area. Focusing on moving healthcare from a curative measure to a preventive system.
Visual collage of extension of health services in the rural area. Focusing on moving healthcare from a curative measure to a preventive system.
In the Hudson Valley, the project focused on the twin counties - Columbia and Greene County. These counties have the lowest access to healthcare facilities but also the lowest physician to patient ratio and higher travel distances for health needs. As we have identified that 84% of the carbon emissions can be reduced through patient preventative healthcare, we look into the health profiles of these counties. In Columbia and Greene county, we see that there is an increase in the aging population and is projected to rise by 2040.
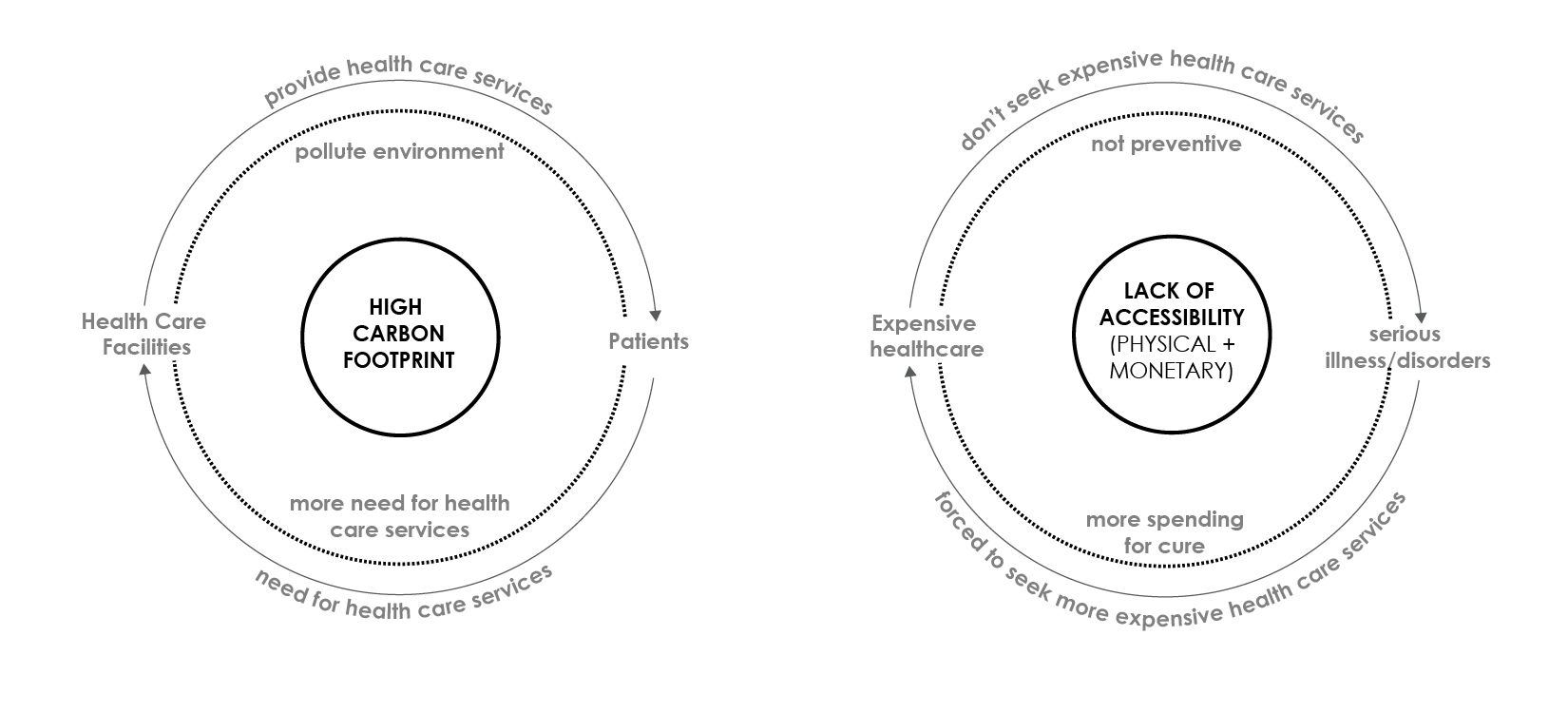
Left: Vicious cycle of Healthcare facilities are high polluters of the environment, in turn making people sicker and more dependent on health facilities.
Right: Another cycle is the lack of physical and monetary access that makes people conditioned to living with the discomfort of disease
According to the health assessment done, there are two main health issues in the county - First, high number of chronic diseases such as obesity. We also see that the community in these regions consume less fresh vegetables, engage less in physical activities and has limited access to fresh food supermarkets. Second, high number of substance use in the middle aged population that also results in mental health issues and social isolation within the aging population in the rural areas.
To respond to the issues of the healthcare system, we propose two strategies that would substantially lower the carbon footprint and reduce health disparities in the Hudson Valley. The first strategy is to extend health services in the rural area by adding health services to public institutions such as fire stations and public libraries. In the twin counties, Columbia Memorial Hospital serves as a sole healthcare provider. As we can see, libraries and fire stations are fairly dispersed in the region. As major health issues in the region are chronic and can be treated through preventative measures, through this strategy we can reduce the carbon impact but also provide health services as closer proximity. The second strategy is the mobile network that would make health services more accessible - scheduled health professional servicing rural areas but also distribution of medications, fresh food and wellness services. As the Columbia Memorial Hospital is a major stakeholder in this process of transition, the idea is to change the perspective of health services. It acts as a promoter of community well being in Hudson and disperses wellness through an additive typology that empowers the role of social infrastructure to spread a wellness network in rural areas.
To respond to the issues of the healthcare system, we propose two strategies that would substantially lower the carbon footprint and reduce health disparities in the Hudson Valley. The first strategy is to extend health services in the rural area by adding health services to public institutions such as fire stations and public libraries. In the twin counties, Columbia Memorial Hospital serves as a sole healthcare provider. As we can see, libraries and fire stations are fairly dispersed in the region. As major health issues in the region are chronic and can be treated through preventative measures, through this strategy we can reduce the carbon impact but also provide health services as closer proximity. The second strategy is the mobile network that would make health services more accessible - scheduled health professional servicing rural areas but also distribution of medications, fresh food and wellness services. As the Columbia Memorial Hospital is a major stakeholder in this process of transition, the idea is to change the perspective of health services. It acts as a promoter of community well being in Hudson and disperses wellness through an additive typology that empowers the role of social infrastructure to spread a wellness network in rural areas.




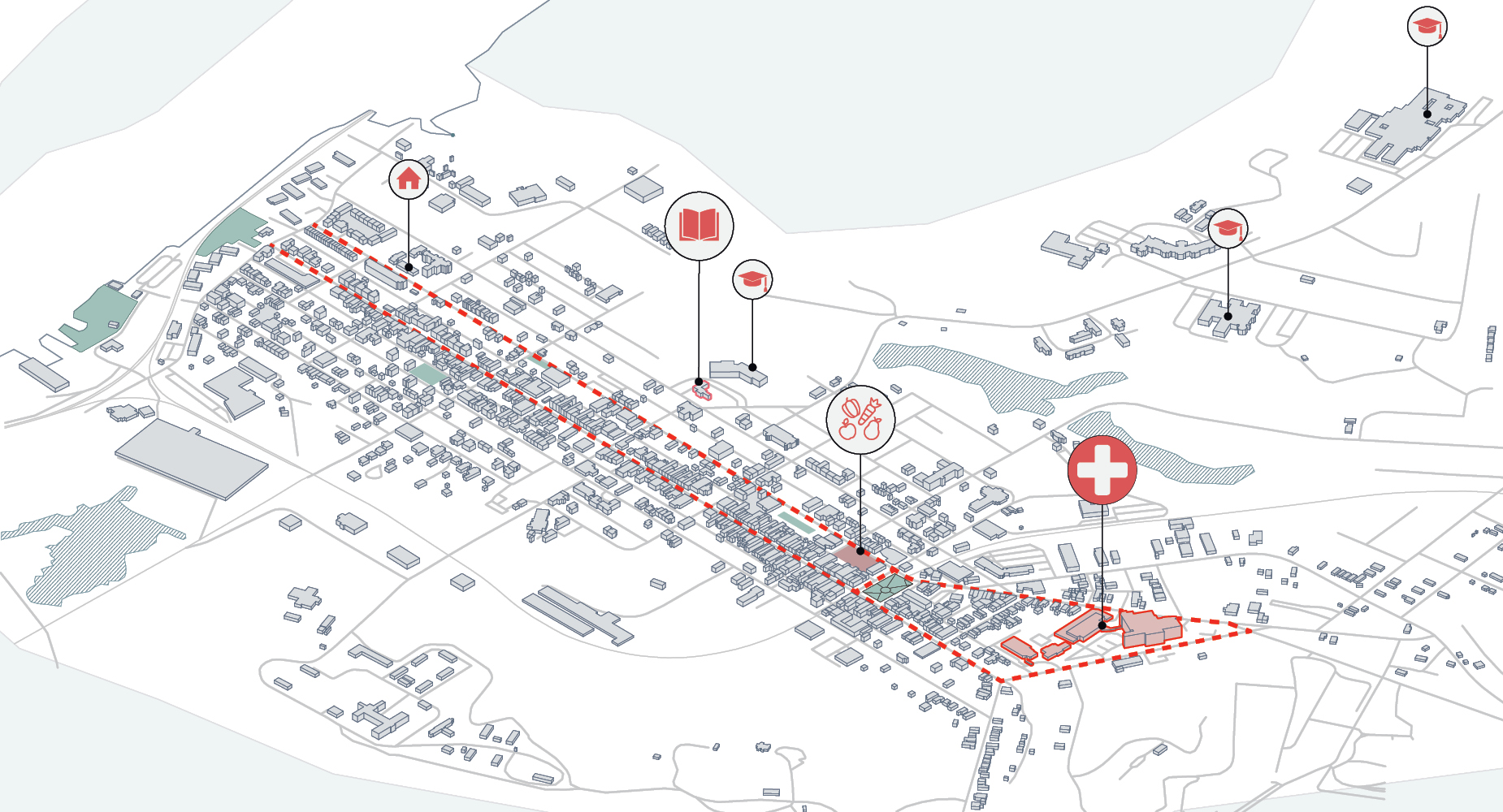 Hudson, Columbia County and its public institutions showing the hospital,school, social housing, library and open vegetable market.
Hudson, Columbia County and its public institutions showing the hospital,school, social housing, library and open vegetable market.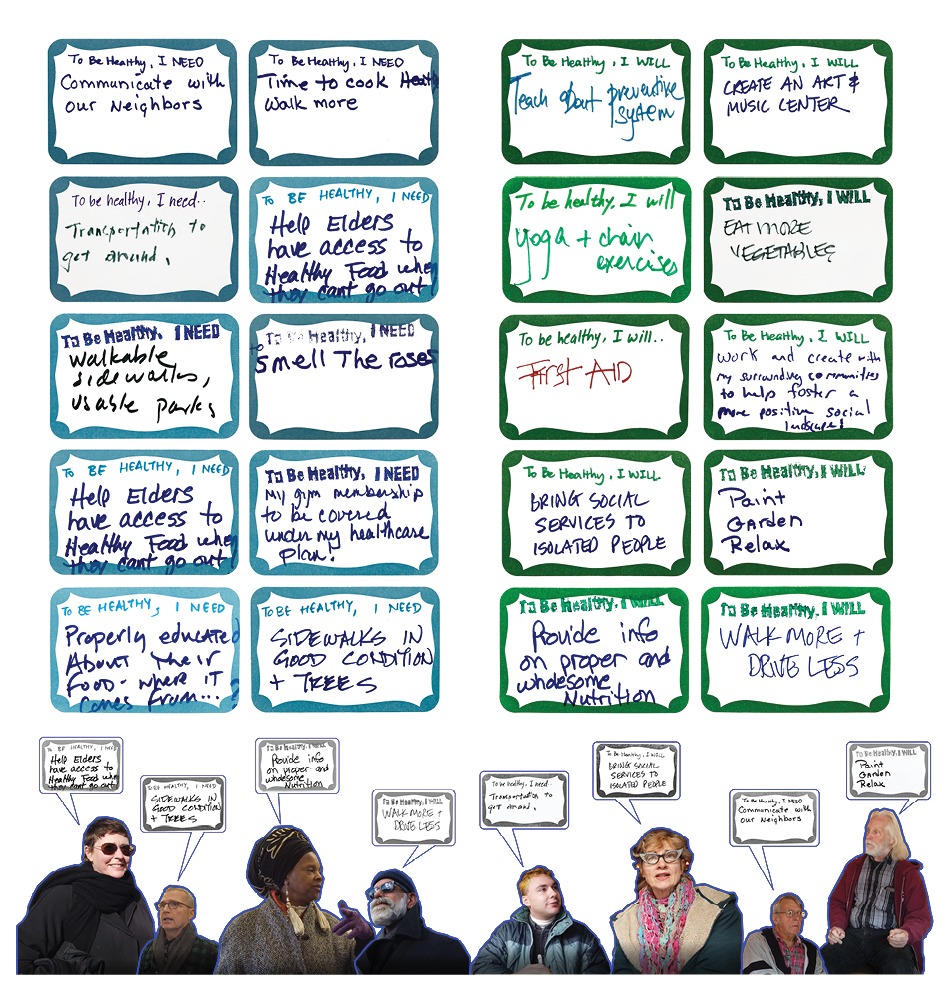 Community engagement exercise conducted to understand the perception if health by members of Hudson and Prattsville community. We wanted to understand what the people need and are willing to do for being healthy.
Community engagement exercise conducted to understand the perception if health by members of Hudson and Prattsville community. We wanted to understand what the people need and are willing to do for being healthy.
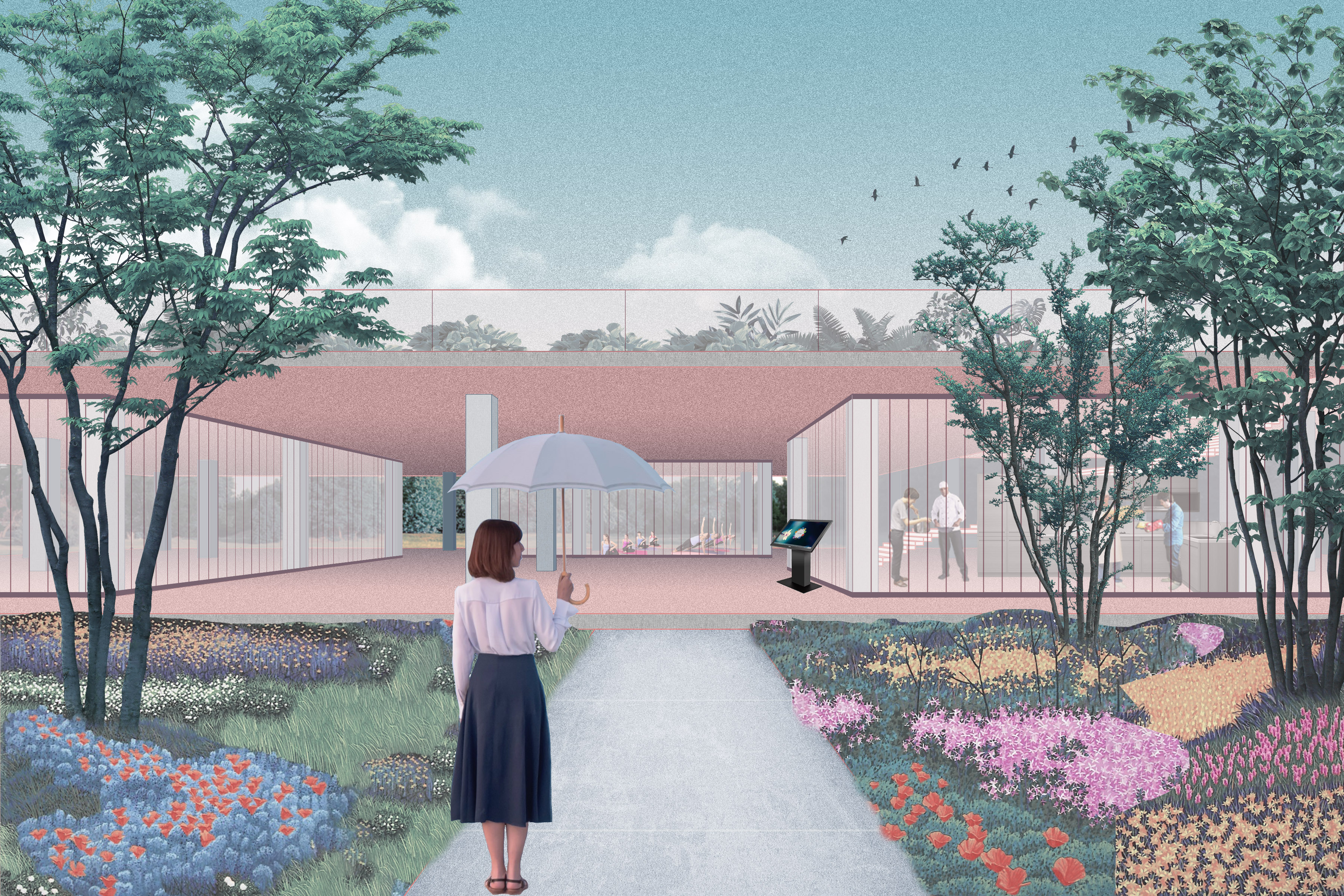
In the Urban areas around CMH in Hudson, Columbia County, we focus on the retrofit of the hospital. We reimagine the hospital as not a place for cure of disease but also as a center of dispersing wellness. Therefore, we propose ‘Hospital as a Park’ strategy considering that in the site analysis we find that there are not many places that promote wellness in the area.
We intend to make the space inviting not just for the people that are sick but also reimagine the space as a form of public space. The overall strategy is to repurpose not fully utilized building by cluster hospitals operational programs into the main functions building and reprogramming other two buildings - Research center to a daycare center, family care and Office building to a wellness pavilion where we have programs such a classroom and training space for librarians and firefighters, telemedicine helpline center, community based programs such as communal kitchen and conference room with a playground.
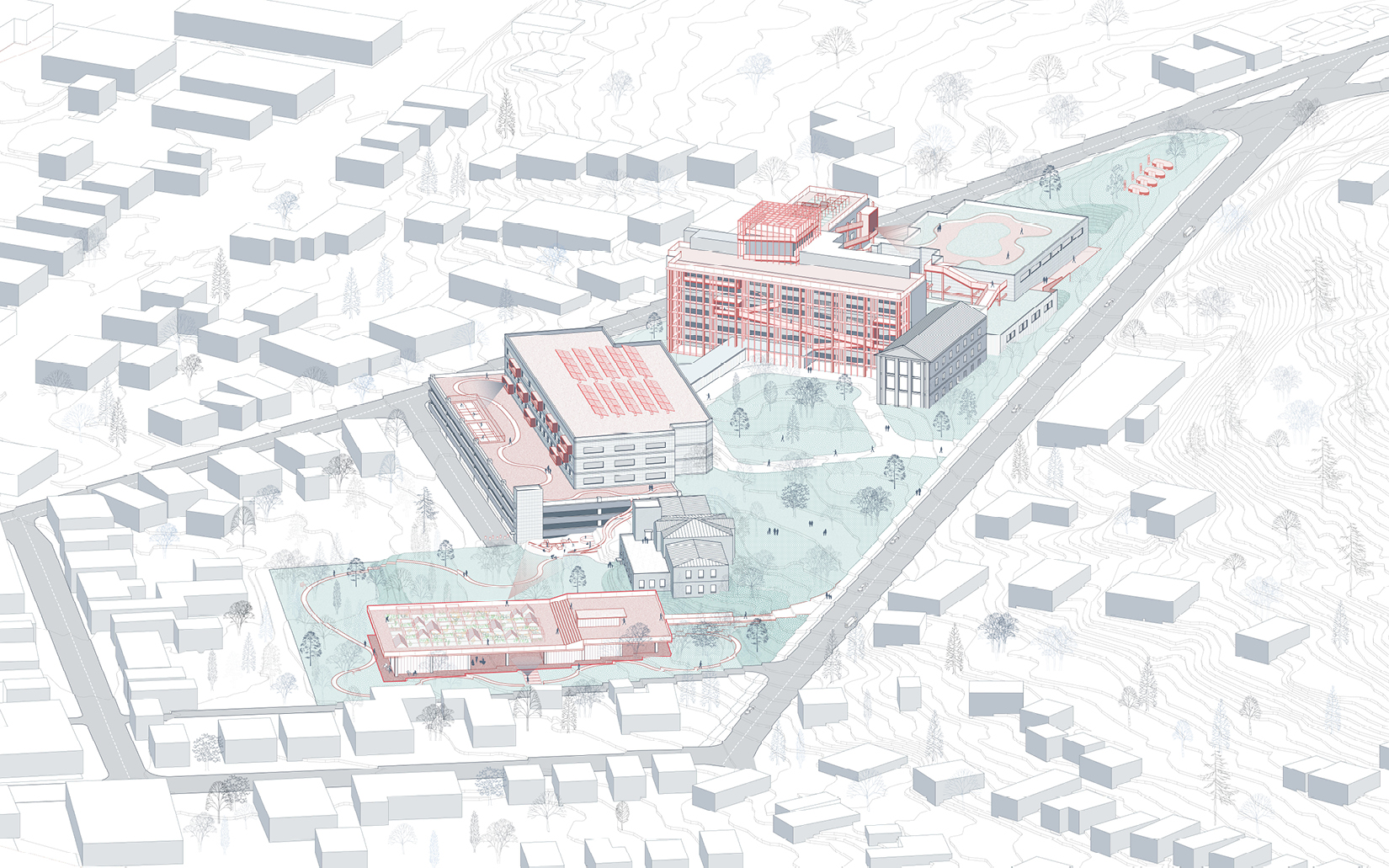 View of ‘Hospital as Park’ strategy considering that there are not many places that promote wellness in the area. We intended to make the space inviting not just for the people that are sick but also reimagine the space as a form of public space.
View of ‘Hospital as Park’ strategy considering that there are not many places that promote wellness in the area. We intended to make the space inviting not just for the people that are sick but also reimagine the space as a form of public space.
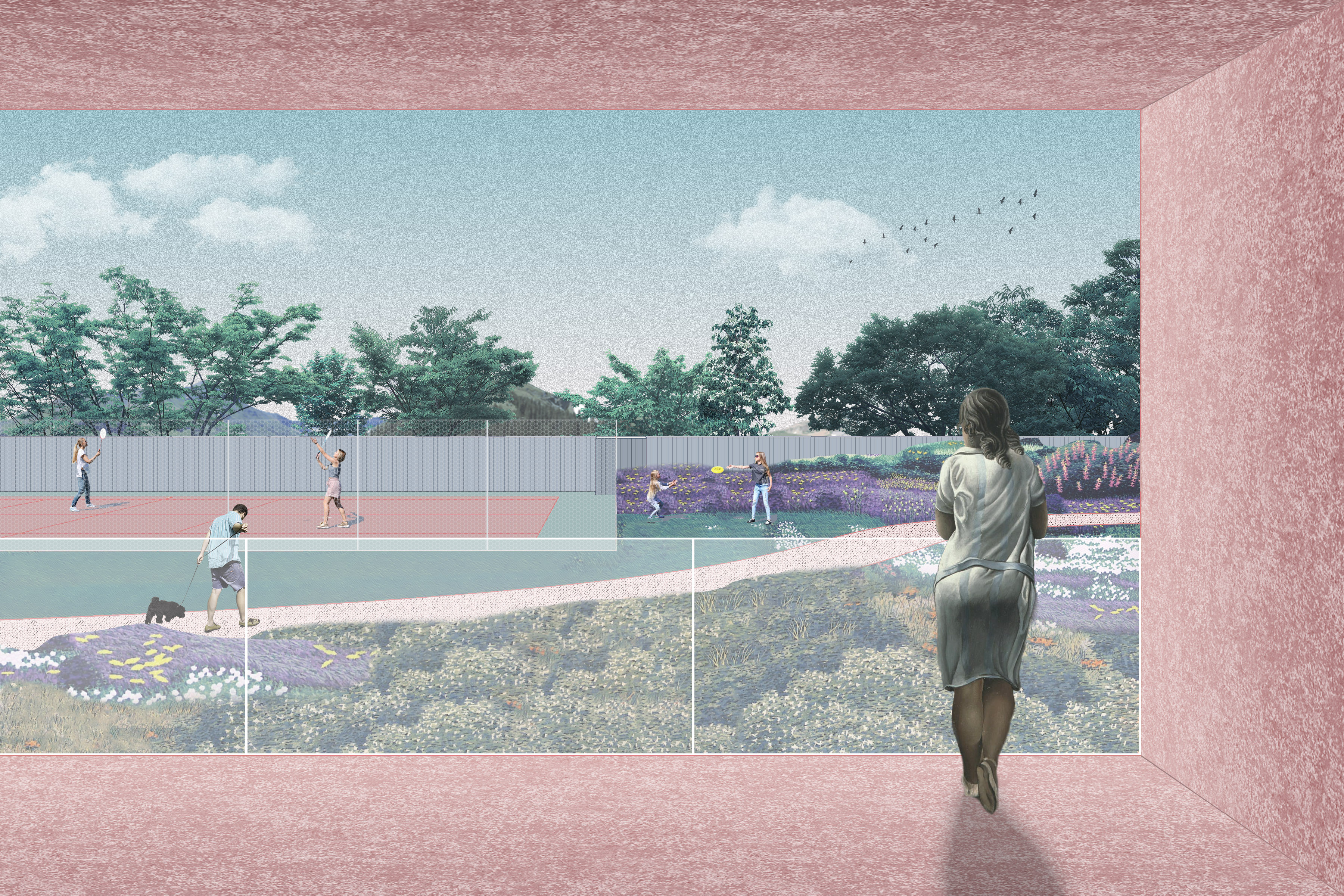
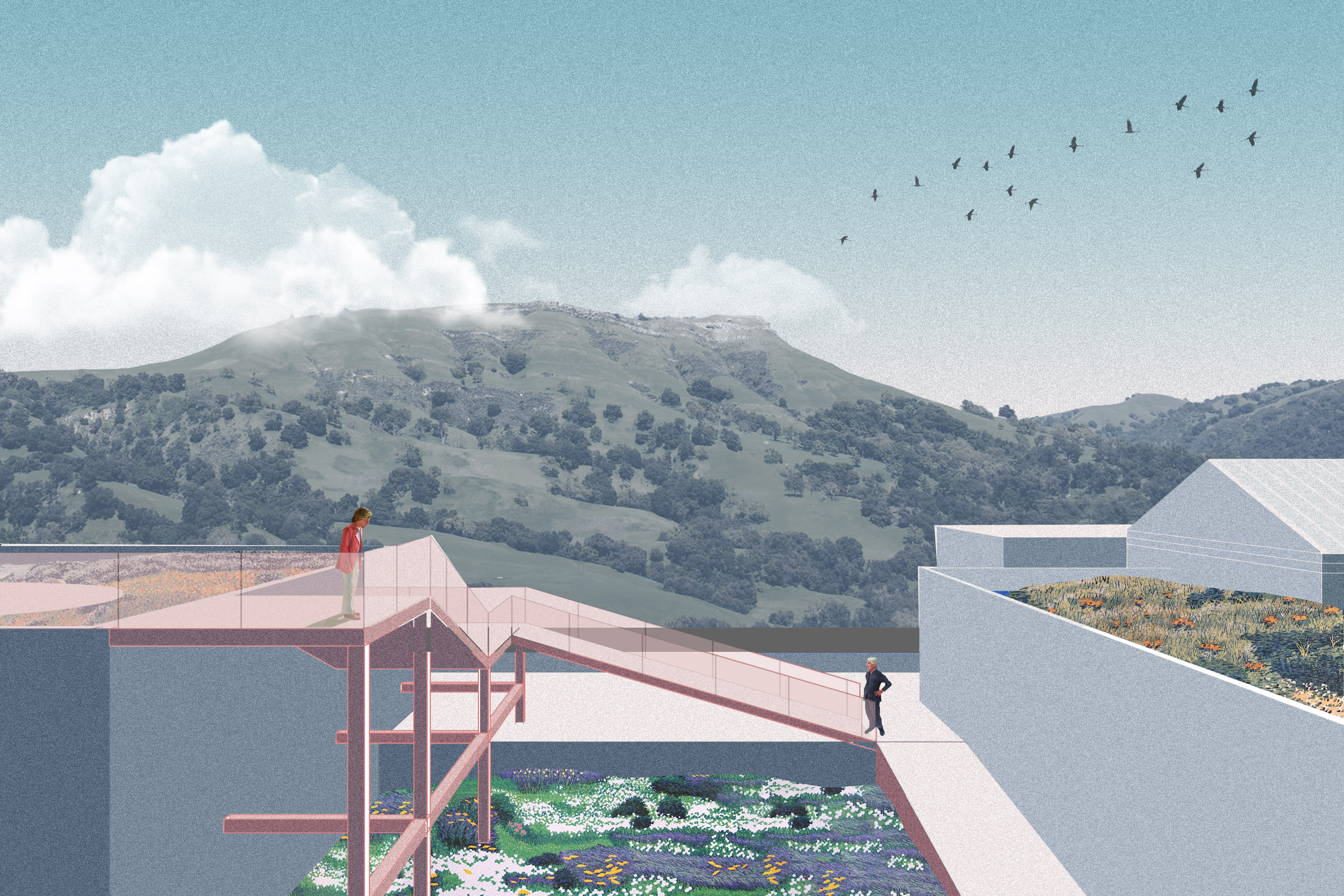
The parking lots on site are converted to green spaces. The park will also have an ongoing health fair where the mobile health vans will be stationed. Residents can get their routine health check up while at the park during scheduled times of the day. To tackle the energy systems that can reduce 12% of the carbon emissions. We proposed to retrofit the facade of the hospital - a double skin facade to make it more energy efficient in terms of heating and cooling. The double skin facade is connected through a series of ramps that form a connection between the buildings. All the buildings have been converted to have farm gardens and solar panels on the roof that help achieve upto 50% of the carbon emissions reduction in the energy systems of the facility.




In the rural areas we propose a shed typology that becomes an attachment to public institutions such as a fire station in Prattsville, Greene county. The Shed is designed to be energy-positive space that provides a high performance, healthy communal environment, while minimizing energy use through careful daylighting and natural ventilation, employing photovoltaic panels to generate substantially more power than consumed. The modular shed can be easily built on site as it has standardized dimensions of 8x16ft and uses 2x4 planks.
By reimagining a dispersion of health services and promoting preventative healthcare programs, we can substantially lower the environmental impacts of the healthcare sector and create an equitable and sustainable model by dispersing wellness.
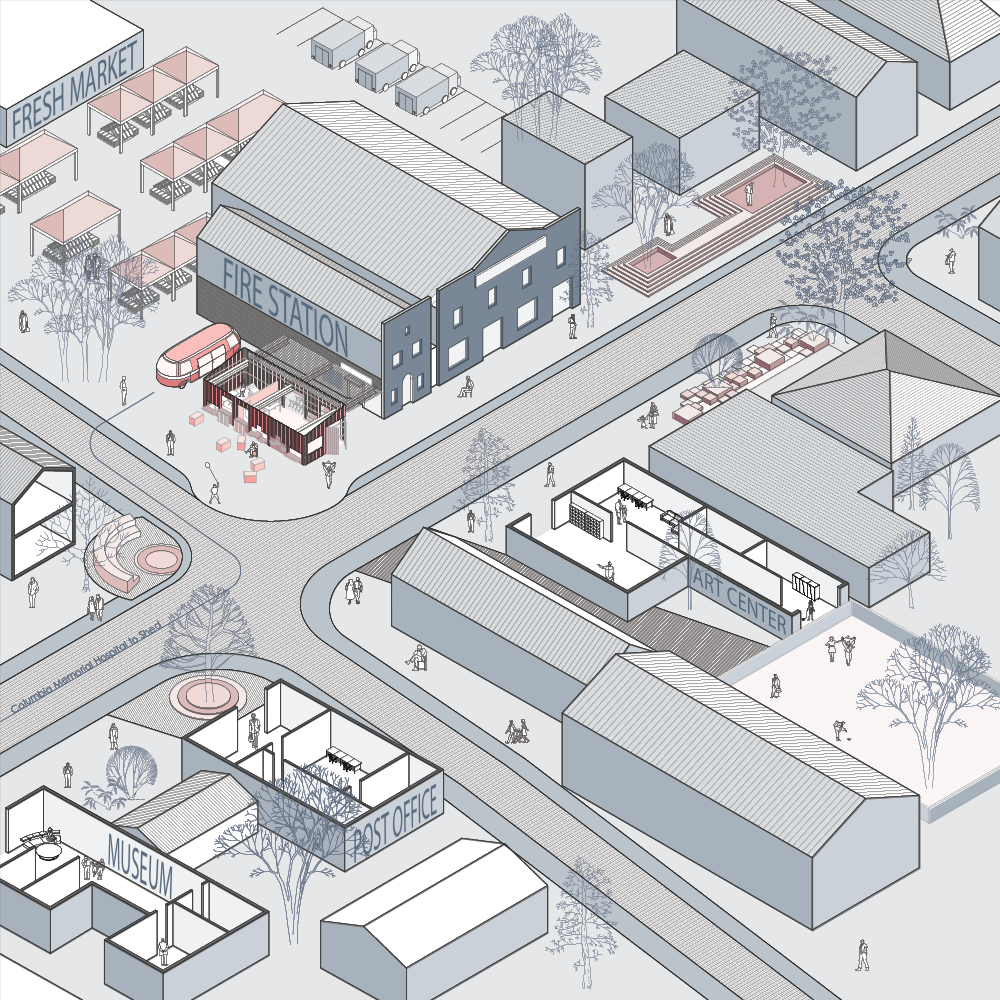
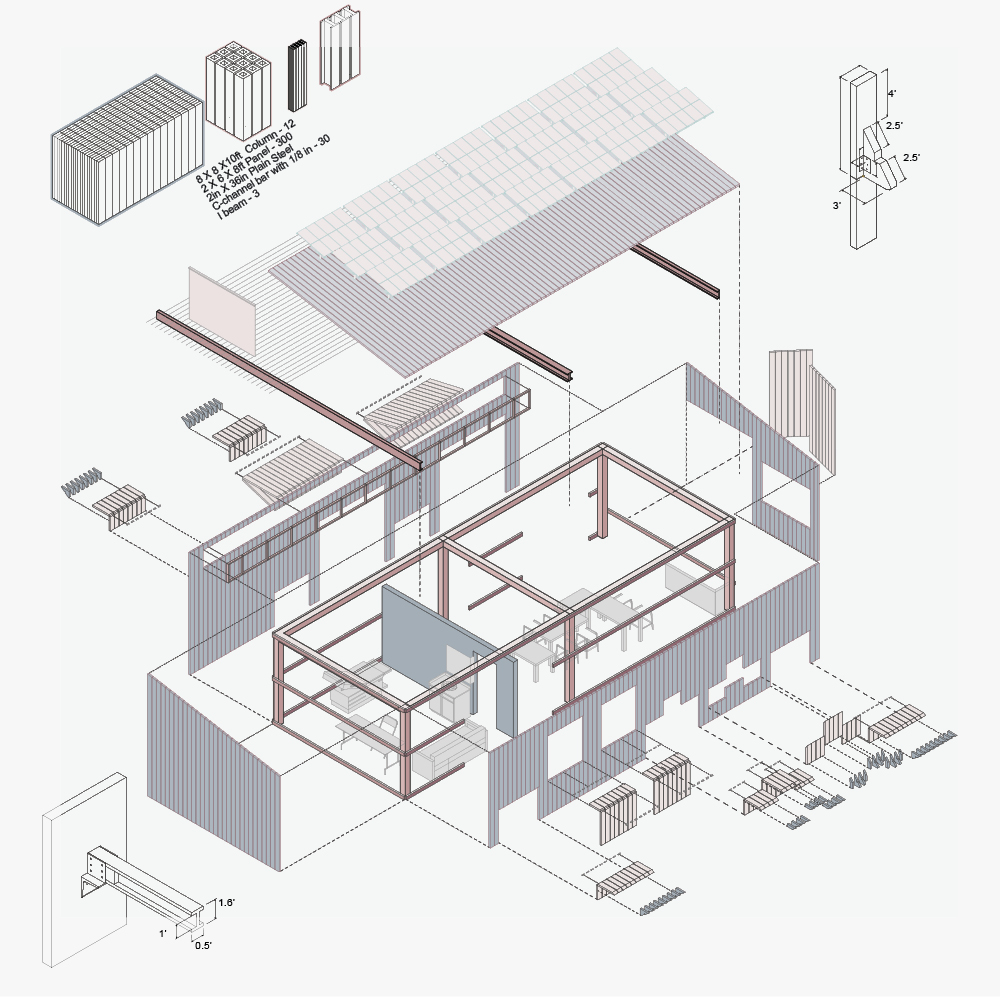
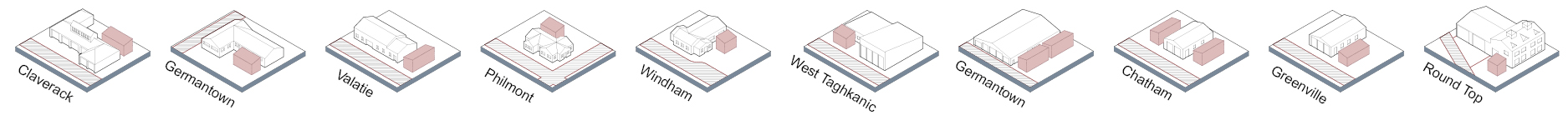
Top: For rural areas we propose a shed typology that becomes an attachment to public institutions such as a fire station in Prattsville, Greene county. The Shed is designed to be energy-positive space that provides a high performance, healthy communal environment. The modular shed can be easily built on site as it has standardized dimensions of 8x16ft and uses 2x4 planks. Bottom: The dispoersion of the shed in different rural town of Greene and Columbia county
This shed will comprise of a storefront health center serviced by a trained firefighter where residents can go for their routine check ups. In the case of Prattsville where the major health issue is social isolation, the shed also serves a communal living room space where programs such as home theatre movie, knitting activities programs that facilitate connections can be carried out. Through the extension of health services in public institutions and dispersing a wellness network in each neighborhood, we strive to make healthcare accessible to all but also promote the healthy living. The mobile health with a certified doctor make routine rounds to these rural areas for further services.Therefore, by reimagining a dispersion of health services and promoting preventative healthcare programs, we can substantially lower the environmental impacts of the healthcare sector and create an equitable and sustainable model by dispersing wellness.





 Dispersing Wellness
Dispersing Wellness